KNEE REPLACEMENT SURGERY
Knee replacement surgery, like all joint replacement surgery, is a very major operation and requires careful consideration and discussion before proceeding.
If, however, the patient and surgeon have come to the decision that there is little alternative, replacement surgery can offer immense symptomatic relief to the patient.
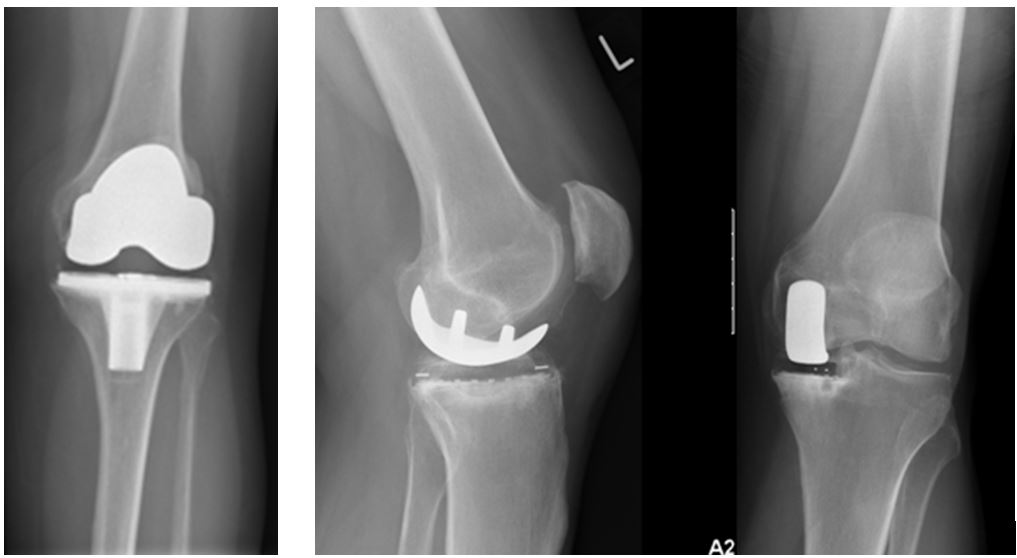
The aim of knee replacement is to replace the deficient joint surfaces (Condyles of the femur and top surface of the tibia) with low friction artificial surfaces (including occasionally the patellofemoral joint if affected). The best function and outcome is in general achieved by restoring mechanical alignment and soft tissue balance.
Knee replacement surgery can be divided into total knee replacement surgery or partial replacement surgery. In both cases, the operation is carried out under general or regional anaesthesia (spinal) and lasts approximately one to one and a half hours.
Total knee replacement surgery involves the replacement of all aspects of the joint with an artificial bearing surface.
Surgery restores the normal alignment of the joint, as well as the smooth articulating surface that has been damaged by osteoarthritis.
Assessment for knee replacement
The basic indications are pain and loss of function.
Selection for surgery should take into account severity of symptoms, the combination or integrated effect of these symptoms and the patient’s motivation to proceed.
Agreed guidance suggests: ‘referral for joint replacement surgery should be considered for people with osteoarthritis who experience joint symptoms (pain, stiffness and reduced function) that have a substantial impact on their quality of life and are refractory to non-surgical treatment. Referral should be made before there is prolonged and established functional limitation and severe pain.
Preparing for Knee Replacement Surgery:
In general, you may be told to:
- Stop medications that increase bleeding – 2 weeks before surgery stop all herbal supplements, weight loss aids, vitamin E and all anti inflammatory medications.
- Fast the night before – No eating or drinking after midnight before surgery; if the operation is in the morning, [or 6 hours before the op]. however, you may brush your teeth or have a few sips of water if you need to take medicines. Discuss the need to take medications such as insulin, heart or blood pressure pills with your doctor or nurse to make sure you don’t miss them.
- Plan for post-surgery rehabilitative care – Total joint replacement recipients may need help at home for the first week, including assistance bathing, dressing, preparing meals and with transportation. Arrange for someone to help you at home. If you need to stay in a rehabilitation or skilled nursing facility, a medical social worker can assist with arrangements.
- Total knee procedures do not require blood transfusion. You will not need to use donor blood or plan ahead to make an autologous donation of your own. There is minimal surgical blood loss. A reinfusion drain is placed in your knee at the at the end of your knee replacement.
- Make sure to take these things with you to the hospital:
- Exercise shoes with closed-in heel and non-slip soles
- Grooming items such as shampoo, toothpaste, deodorant, etc.
- A list of medications you are currently taking at home, including the name, strength and how often you take each medication.
- A list of allergies (to food, clothing, medicine, etc.) and how you react to each one.
- Glasses, hearing aid, and any other items you use every day [Short gowns, pyjamas, underwear, socks/stockings and one set of street clothes to wear home.
- Leave jewellery, credit cards, keys and check books home. Bring only enough money for items such as a newspaper, magazine, etc.
THE OPERATION
At surgery, an incision measuring about 8 inches long will be made on the front of your knee. The surgeon will remove small amounts of worn bone from the lower end of your femur and the upper end of your tibia so we have flat surfaces to fasten your new prosthesis to. Some patients require computer navigation to ensure optimal fit. Once your surgeon is satisfied that the prosthesis fits properly it will be secured in place.
When you surgeon is ready to close the incision, a tube may be inserted to drain excess fluid. This is usually removed the first day after the operation.
What are the complications of this operation?
As with all operations, it is very important that you fully understand the ‘pros’ and ‘cons’ before electing to proceed with surgery. Whilst the benefits are clear, time must be given to discuss ‘what can go wrong’.
The main risks of knee replacement include:
- The main complication post-operatively is that of infection. It occur less that 1%. In such cases the patient will develop a temperature, possibly with rigors and inflammation and redness of the wound in the early stages.
- Deep Vein Thrombosis(DVT) Or blood clot, leading to pulmonary embolism (blood clot to lung) This risk is very small, less than half of one percent (0.2-0.4%).
- Nerve or blood vessel damage during surgery.
- sensitive scar with permanent numbness on the lateral aspect of the scar.
- Chronically painful knee replacement (of unknown cause).
- urinary or chest infection.
These may prolong your stay in hospital by a few days. They will occur in 2-4% of cases.
Whilst all of these complications are extremely rare, they can occur.
How long will I be in hospital for?
Patients usually stay in hospital for two days but this could be extended up to one week. During this time you will have daily physiotherapy.
Patients are ready to leave hospital when they can:
* Bend the knee to a right angle.
* Manage stairs independently.
* Walk independently with a stick.
After knee replacement
- In hospital, postoperatively, early knee movement, within the first 24 hours, is encouraged with:
- Good analgesia. Often patient controlled methods. Epidural methods also commonly used.
- Physiotherapy. Continuous passive motion machine may be used. Exercises taught. Most patients walk on the 2nd postoperative day.
- Early discharge is encouraged after 2 days only if:
- Wound healing is satisfactory
- Mobility is satisfactory
- Knee flexion of 90 degrees is achieved
- No complications have been identified.
- Orthopaedic follow up is usually at about 6 weeks in outpatients.
After you go home you should continue exercising to strengthen and improve the range of motion of your new knee.
Although you should be able to get back to light work (such as a desk job) in about 6 weeks, it may take longer (3 months) to start doing more active work.
Don’t engage in strenuous activities like jogging, running, or active sports until your surgeon says so.
If you have any of the following after returning home call your surgeon or the hospital who will contact your surgeon:
- Fever or high temperature.
- sudden shortness of breath or chest pain.
- increase in knee pain.
- excessive warmth, redness, or discharge from the incision site.
- swelling or pain of the calf or leg.
When and who will take my stitches out?
Sutures/clips in the skin will be removed at two weeks by your GP or at the hospital if preferred.
Will I require physiotherapy following my op?
You will need to see a physiotherapist reqularly within the first few weeks post-op.
When do I see My surgeon again after hospital discharge?
All patients will be reviewed after six weeks to check on their progress.
The main concern is to ensure that the wound is healing well and that the swelling is beginning to reduce. However, you should expect the knee to be swollen sometimes for several months.
When do I recover fully from surgery?
Recovering from a total knee replacement operation takes time; sometimes it takes as long as a year for the knee to feel comfortable again.
Interrupted sleep, unfortunately, is normal in the first three months after such major surgery and you should be prepared for this.
When can I return to other activities after knee replacement?
- Return to work. This depends on type of work, but may take up to 6 weeks.
- Driving: if left knee replaced and automatic, then driving can be resumed as soon as 2 week after surgery. If right knee replaced 6 weeks off driving is to be expected.
- Travelling. Measures to prevent thromboembolic complications are recommended. We recommend avoid flying for 6 weeks.
- Sleeping positions. Sleeping on back, side and stomach is safe any time.
- swimming is recommended, usually from the time sutures are removed (about 2 weeks).
- Dancing, golf , cycling (level ground) 6 weeks
- Activities which stress the joint should be avoided for 12 weeks ( for example: tennis, squash, jumping, skiing, jogging).
How long will my new knee last?
15 years, 90% of replaced knees will still be functioning correctly.
Minimally Invasive Surgery (MIS) for Knee Replacement


Minimally invasive surgery is improving patient’s lives after knee replacement. Many patients have less post operative pain, recover faster and are hospitalized for only one or two nights. The benefits derived from minimally invasive surgery are due to the fact that no incision is made in the quadriceps tendon (the large muscle on the front of the thigh) and the procedure is done through as small of skin incision as is possible (depending on individual patient factors) causing less traumas to the soft tissues. We combine MIS technique with computer navigated instrumentation for the most precise placement of your new knee.
Computer Assisted Surgery (CAS) is one approach to reduce surgical errors and improve surgical outcomes associated with knee and hip surgery.
Computer assisted orthopedic surgery is defined as techniques that enhance identification of surgical anatomy thereby improving surgical accuracy. These computer based tools increase the repeatability and accuracy of surgical procedures and should improve quality control in orthopedic surgery.
Computer Navigation utilizes an operating room based computer and infra-red transducers pinned to the thigh and shin bones. The patient’s unique anatomy is mapped and displayed on the computer screen. This real time anatomic data is used to plan and verify bone cuts for precise implant placement.
Potential advantages of CAS are:
- Enables the surgeon to create accurate and reproducible bone cuts helping to ensure accurate placement of Total Knee implants.
- Greatly reduces possibility of MIS technique component mal-positioning.
- Vital for complex TKR when unusual bone deformities are present.
- Valuable tool when performing revision total knee replacement.
Potential disadvantages of CAS are:
- Time in operating room could be longer due to setup, calibration and usage of computer.
- Navigation Pin breakage, femur or tibia fracture/stress fracture, prolonged bleeding/drainage from navigation pin sites (all rarely occur).
- Computer or tracker malfunction could require conversion to traditional total knee instruments (rarely occurs).

What is minimally invasive surgery of the knee joint?
This term is applied when the surgeon selects a method in which the tissues about the knee joint are disturbed or cut in the least amount possible to perform the surgery.
In years past, the use of arthroscopic-guided surgery in the knee joint was considered minimally invasive as it allowed the surgeon to perform a great deal of the surgery through small incisions. Visualization through the arthroscope decreased the need for large incisions or any incision at all. A majority of ligament reconstructions and other knee repairs are now performed by surgeons trained in these arthroscopic techniques.
Knee replacements are now being performed using minimally invasive types of techniques. The instruments used during the procedure are smaller and the incisions are also smaller resulting in fewer disturbances of the soft tissues. The computer-assisted surgical technique allows in some cases the ability to use smaller incisions as the computer provides virtual visualization or navigation during the procedure.
Whenever the surgeon can minimize the incision or disturbance of soft tissues, generally there will be less pain after surgery and a more speedy recovery. Less pain medication is necessary and the patient is out of bed sooner and more frequently. The rehabilitation process is easier and the muscles regain their function faster. This has been proven in all aspects of knee surgery when these lesser invasive techniques have been applied.
How long will I be in the hospital?
Patients normally stay in the hospital for 2 days after a knee replacement. The physiotherapists make sure that the patients are able to walk independently, with the help of crutches or walking frames, and negotiate stairs before being discharged from the hospital.
Is blood transfusion common after a joint replacement?
The chance of receiving blood transfusion after a knee replacement is less than 10%. In a fit and healthy person with high pre-operative haemoglobin the chances of blood transfusion is very low.
What is computer-assisted knee replacement?
A computer with specialized software is used in the operating room to assist the surgeon to achieve proper placement and alignment of the knee prosthesis. The system provides instant information on the boney alignment of the knee joint, the function and tensions of the ligaments required for knee stability, and the special cuts that must be made in the femoral and tibial bones to achieve a precise placement of the prosthesis.
