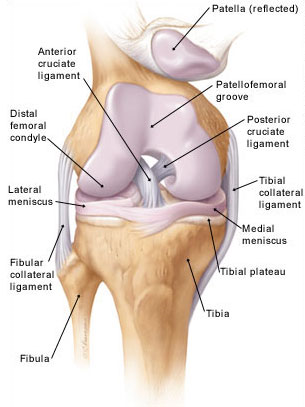
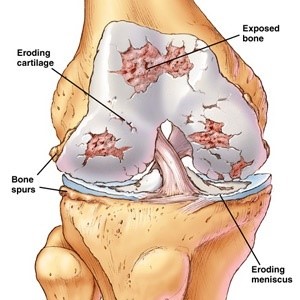
The knee is a joint articulation formed between the top of the shin bone (tibia) and the bottom of the thigh bone (femur).
Like all large joints in the body, the joint surfaces of the knee are covered in what is known as hyaline cartilage. This cartilage protects the knee against stress and absorbs shock.
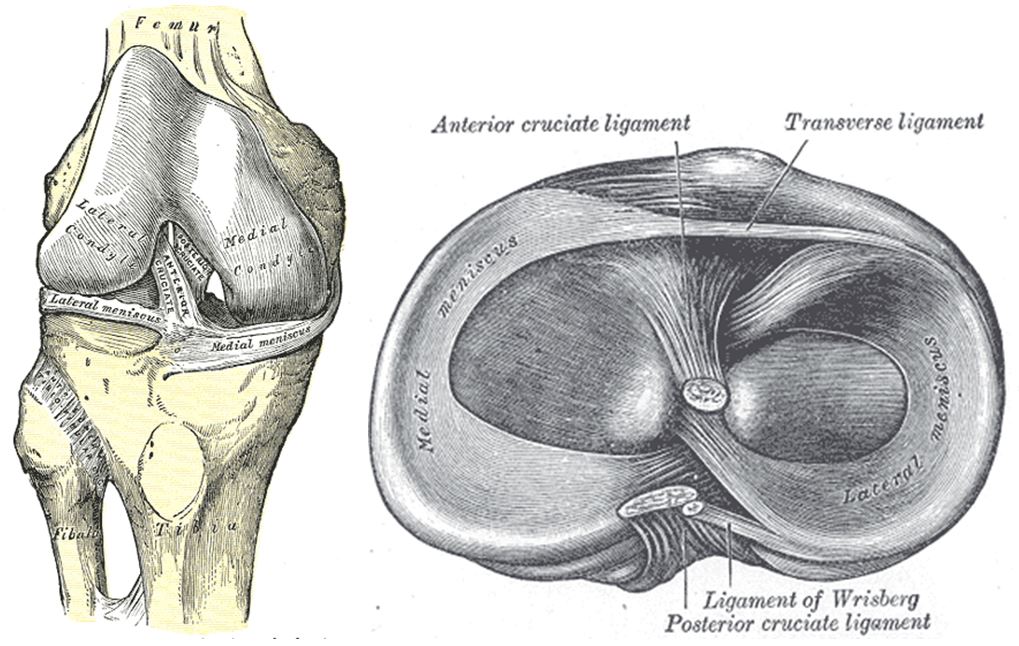
Knee anatomy
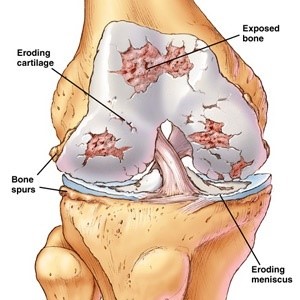
As we age, this “cushioning” cartilage can wear away naturally. Also, damage can occur prematurely due to infection or trauma. When this occurs naturally, as part of the ageing process, it is known as osteoarthritis.
As this cushioning cartilage thins, the knee has less protection against shock and the bone ends can become “injured” by day-to-day activities such as walking. The underlying bone can become inflamed, which in turn can produce aching pain.
The symptoms of osteoarthritis include:
• aching pain within/around the knee
• occasional swelling
• stiffness after activity

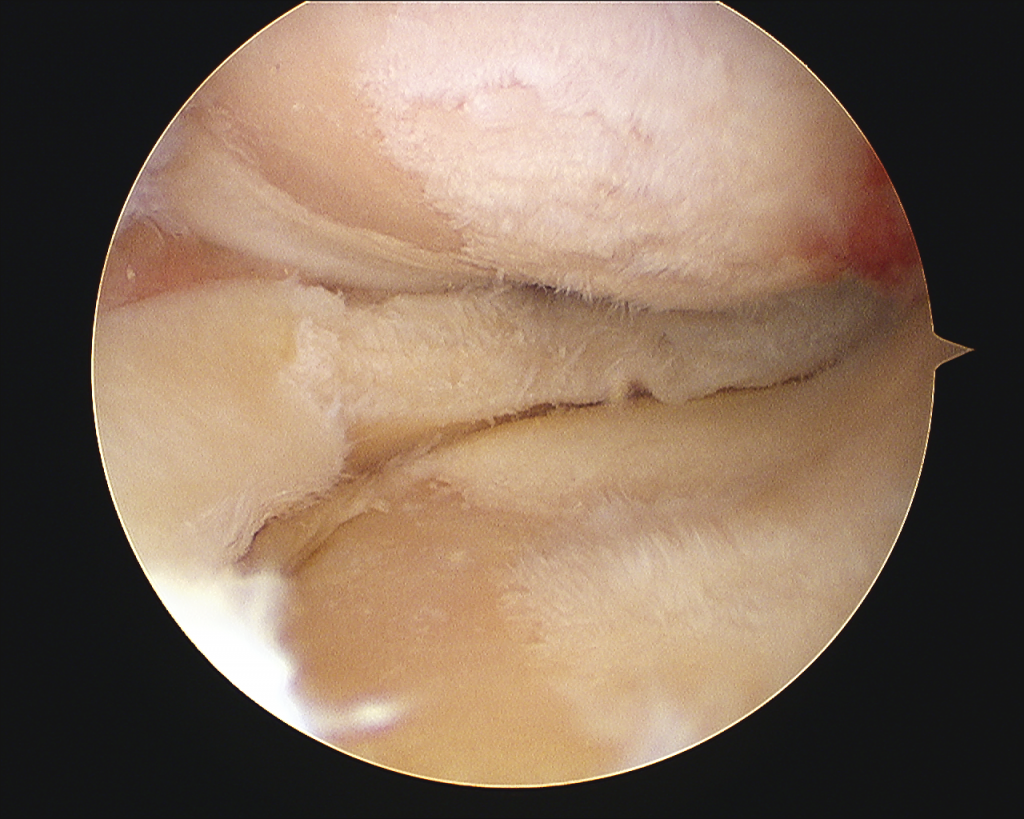
Arthroscopic picture of knee with advanced arthritis
Knee Arthritis:
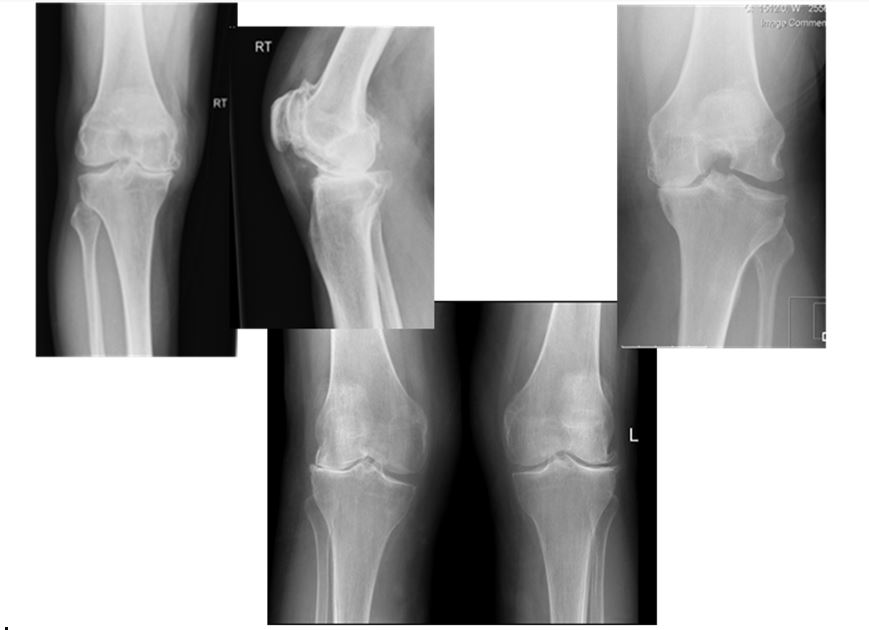

Patellar arthritis
TREATMENT OPTIONS of knee arthritis:
It is preferable that osteoarthritis is treated conservatively (without surgery) for as long as possible. However, the need for replacement of the joint may ultimately become inevitable, due to deterioration in the condition of the joint leading to increased disability and pain.
CONSERVATIVE TREATMENT
Conservative (non-invasive) treatment of knee osteoarthritis involves a combined approach:
- Adequate pain management. This should include oral drugs (non steroidal inflammatories etc).
- Weight loss
- Physiotherapy to help with muscle strengthening, gait, patient education, joint mobility, walking aids.
- Walking aids (shoe adjustments, bracing of joints etc).
- On occasions, some patients will be considered suitable for a series of hyaluronic acid injections into the knee as a part of the treatment referred to as viscosupplementation. These injections help to lubricate the degenerating joint surface and can be very effective in a small majority of ‘early’ cases.
- There is a role for the use of injected steroid into the knee when/if acutely inflamed but is usually considered in rare episodes of extreme discomfort.
Hopefully, with conservative management, patients can avoid the need for surgery for many years after the onset of arthritis.
KNEE REPLACEMENT SURGERY
Knee replacement surgery, like all joint replacement surgery, is a very major operation and requires careful consideration and discussion before proceeding.
If, however, the patient and surgeon have come to the decision that there is little alternative, replacement surgery can offer immense symptomatic relief to the patient.
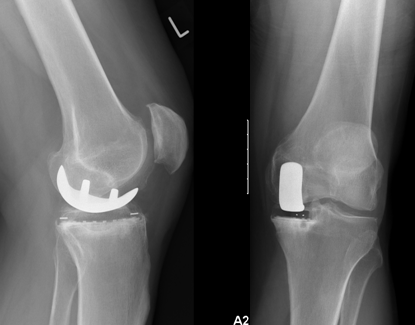
The aim of knee replacement is to replace the deficient joint surfaces (Condyles of the femur and top surface of the tibia) with low friction artificial surfaces (including occasionally the patellofemoral joint if affected). The best function and outcome is in general achieved by restoring mechanical alignment and soft tissue balance.
Knee replacement surgery can be divided into total knee replacement surgery or partial replacement surgery. In both cases, the operation is carried out under general or regional anaesthesia (spinal) and lasts approximately one to one and a half hours.
Total knee replacement surgery involves the replacement of all aspects of the joint with an artificial bearing surface.
Surgery restores the normal alignment of the joint, as well as the smooth articulating surface that has been damaged by osteoarthritis.